Real World Evidence Evidence & Data Partnerships
This year real patient data will change healthcare.
Substandard EHR Systems Help Vendors, Not Patients
Authors of a survey highlighting the difficulties of digitizing the US health system warn that the results “should be of concern to policy makers” as “significant progress needs to be made before such systems are believed to be usable by most physicians”.
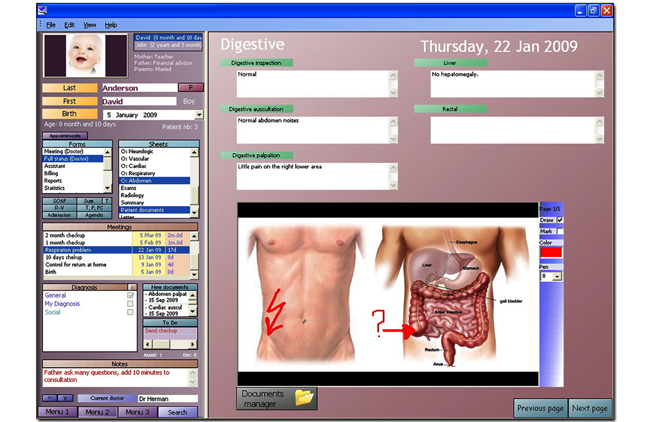
Fewer than 10 per cent of doctors used electronic health records (EHRs) last year to US standards, according to the report published yesterday by the journal Annals of Internal Medicine (AIM). And while this meagre amount of physicians used electronic systems that fulfilled the criteria for “meaningful use”, less than half all those surveyed (44 per cent) had any system in place at all. The researchers surveyed 1,820 primary-care and specialty doctors over a period from late 2011 to early 2012. A third or less of participants had a digital system for tracking referrals, generating reports on quality of care, sending patients reminders for preventive or follow-up meetings or generating lists of those who had missed appointments or were overdue for care.
Moving away from paper
In 2009, US Congress passed the Health Information Technology for Economic and Clinical Health Act. Health care providers were encouraged to make the move to electronic systems of “meaningful use” through monetary incentives – punitive action was also an option if the shift to digital was still not made. The ‘carrot and stick’ tactics have worked to some extent.
New data released last month (22ndMay) by the Department of Health and Human Services (HHS) shows that more than 50 per cent of doctors and 80 per cent of hospitals have received enhanced federal funding for achieving “meaningful use” of digital records. And over half of doctors in the US have now opted for EHRs in lieu of paper-based systems.
The Obama administration’s support for EHRs, spending about $15 billion in the last three years to help doctors and hospitals go digital, naturally attracted the attention of entrepreneurs and venture capitalists. But while the criticism of electronic record vendors is predominant, it’s nonetheless important to acknowledge the very real benefits for patients in streamlined processes and efficient data collection. Test results, procedures undertaken and information gaps in healthcare are significantly better analysed from electronic records than sourced from a manila folder. Recent examples reported in the media include family medicine specialist, Dr. Jen Brull, who alerted relevant patients to have colorectal cancer screening; and the difference in the aftermath of natural disasters as regards the protection of health records – from Hurricane Katrina to the tornado in Oklahoma City.
Qualifying the benefits
Indeed, the migration from paper is not the issue that is causing much heated debate around the implementation of EHRs in the US. In fact, this latest study actually found a rise in the number of physicians using computer records from 34 per cent in 2011. Rather, the contention stems from the issues caused by the government's incentive program and the seemingly steadily increasing financial and operational costs involved in rolling out, using, and paying for EHR systems. And of those doctors surveyed for the AIM report, more than 50 per cent found it hard for their systems to meet some or all of the “meaningful use” standards, which the federal government requires for subsidy payments.
Last September, the same month an article for the Wall Street Journalcontending that EHRs don’t save money as claimed was published (by professors Stephen Soumerai from Harvard Medical School and Ross Koppel from the University of Pennsylvania), the federal government accused healthcare providers of “upcoding”, that is, claiming to have provided a medical service or procedure when it wasn’t really performed. Physicians were suitably incensed at the accusation and the implication that those billing through EHRs would be more closely monitored for possible fraud.
Adding fuel to the fire in November, HHS inspector general (IG) released a report indicating that the EHR incentive program administered by the Centers for Medicare & Medicaid Services (CMS) was “vulnerable” to fraud. While the CMS agreed with the IG that it needed to start verifying that healthcare providers met the meaningful use criteria, it sided with discontent healthcare providers about having to offer excessive proof.
Perhaps the greatest blow for the Obama administration came in January this year when RAND published a new EHR study that basically renounced one of its key studies from 2005 (paid for by large system vendors) that was a major point behind selling Congress on the EHR initiative. The latest RAND study admitted that it was overly optimistic and has since avoided putting any numbers on how much EHRs reduce (or increase) costs. This latest AIP report shows the federal government needs to set higher standards for vendors, said Koppel, if the systems are to fulfil their promise – and not simply expand the vendors’ bottom lines.
“What these findings illustrate, unfortunately, is that efforts intended to improve quality and reduce health-care costs instead seem to have stimulated sales and implementations of systems that do not work very well,” wrote Koppel in an accompanying editorial “[W]e must shift from cheering health information technology implementations to demanding health information technology utility.”
Real World Evidence Evidence & Data Partnerships
This year real patient data will change healthcare.
