Real World Evidence Evidence & Data Partnerships
This year real patient data will change healthcare.
Electronic Medical Records: Are We There Yet?
With electronic medical records seeing a greater adoption than at any time in the past 30 years, Brian Wells AVP for Health Technology & Academic Computing at Penn Medicine answers our questions on the viability of widespread adoption.
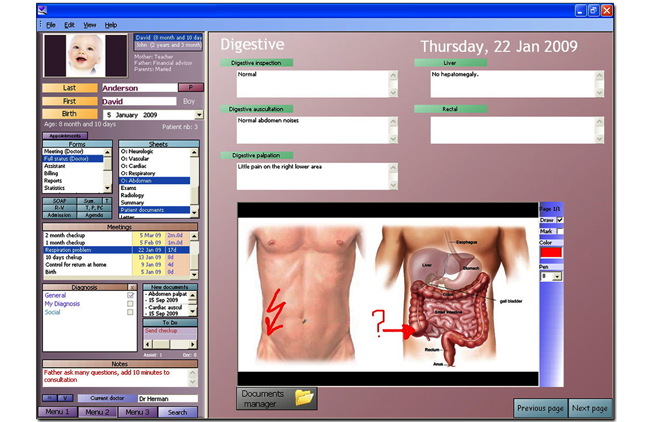
Implementing EMR systems for data capturing is a goal of many of today’s healthcare providers. Hospitals are utilizing technological advances to develop EMR systems for millions of patients and they are interacting with the pharmaceutical industry for innovation. But what are the issues facing the industry in the face of such a radical upgrade? Brian Wells AVP for Health Technology & Academic Computing speaks to Zuzanna Fiminska about what he has learned during his work at the University of Pennsylvania Health System.
“Currently, across the US health system, electronic medical records have not evolved far enough when it comes to ensuring continuity of care. That's something we need to work on as a national healthcare system. In my 33 years of being in healthcare IT, this area really hasn't gotten that much better,” says Wells.
“The country has moved forward in making our systems electronic, and storing the data electronically, but we haven't done much to make the data easy to share. And until we do that, coordination of care is mostly a manual effort between human beings sharing documentation between institutions.”
“Part of the rule of meaningful use is that you need provide your data in mapped standards, so there is a lot of need for people to standardize lists of values”
How this works
“Part of the rule of meaningful use is that you need provide your data in mapped standards, so there is a lot of need for people to standardize lists of values. The goal is to ensure that the procedures, medications and services are standardized across different providers, viewing all prescribed medications on one screen, etc. If you've fallen ill and you go to hospital, it may be very hard at some care offices in the U.S. to find out how you've been treated by either your current doctors, or any previous hospitalization. Even if we talk to those physicians and get that data from them, it may be difficult to take that data and use it in a way that we can automate clinical decision support. It's probably going to come over as free text, and we'll have to read it, but we won't be able to use it, or store it, or put those discrete values in our system.”
“There are hundreds of vendors who provide systems from the small practices to the largest institutions. They provide the same functionality, but they have different methodology, different look and feel, and different screen design”
Getting there
“Implementing those systems is a lot of work. It takes a lot of money; it takes a lot of smart people who know how to run this software, who know how to build the infrastructure the technology runs on, it takes a lot of sharing of the ideas and concepts, and a lot of collaboration amongst the physicians. It's not a small undertaking, it takes many years and costs [are high breaking down into] hardware, generally infrastructure, people, and then software vendor, licensing and support.”
“It's a fragmented market in many ways. There are hundreds of vendors who provide systems from the small practices to the largest institutions. They provide the same functionality, but they have different methodology, different look and feel, and different screen design. The system could be standardized, but every hospital implements it slightly differently, each hospital has its own list of services and medications they put on a formulary, so those lists are generally not matched to national standards or even state standards for Health Information Exchange, it’s difficult to exchange data on patient from one place to another because of the way the software was implemented, not necessarily because of the way the software was built by the vendor.”
“An ideal system would have a good solution to interchange data and store data that's been interchanged, so if you come in and you say that your records are in a hospital in Kansas, we should be able to connect to that hospital online in seconds, and then that data would be stored in our system, looking exactly like the data we've collected on you while you were in our hospital. That would be ideal. You could do that if there were national standards, if every vendor had a system for storing data and sharing data, and if there were a national network that connected [hospitals and clinics] together in a secure and reliable way. And that's a lot of what we're trying to do as part of meaningful use, but that's still going to take a few years.”
“Data is also used as a part of real-world-evidence that allows us to assess treatments that have been approved and are already being used”
Data matters
“All our patients sign a release allowing us to collect their data and store it, and we have to store it on our servers in an encrypted way and keep it encrypted while it moves around, to make sure we have firewalls, that people who have access to it are authorized to do it, to keep track of who's got access to that data. However, as we move into the world of data sharing, and the concepts of accountable care where providers take responsibility for the overall treatment, there's going to be a need for people to see more data, so it's going to be difficult to have 100% privacy while we're trying to provide effective care. Those two concepts are at odds with each other.”
“The Attorney General's office and the Office of Civil Rights in the Federal Government have taken on the enforcement aspect, and now they're beginning to check those things and doing audits making sure that people are compliant. or be subject to serious fines and legal ramifications.
“Data is also used as a part of real-world-evidence that allows us to assess treatments that have been approved and are already being used. We're still getting there, we haven't really collected a lot of detailed outcomes yet, like pain scores, or quality of life, but i think we're now starting to have the time and technology to capture that information, so those outcomes can be considered as part of care patterns, and then we can ascertain which care patterns provide the best outcomes.”
Brian Wells will showcase what he has learned from his EMR work at the Penn Medicine – University of Pennsylvania Health System at the Real World Evidence 2013 event next month in Bethesda, Maryland. For more information or to find out who else will be presenting, visit the official website.
Real World Evidence Evidence & Data Partnerships
This year real patient data will change healthcare.
