Advancing Delivery of Paediatric Chemotherapeutic Drugs Via Nanotechnology
New research highlights the true potential of nanoparticles to deliver chemotherapy to children in a form targeting only cancer cells and significantly reducing the side effects resulting from traditional drug delivery methods.
Reported in the latest issue of Molecular Pharmaceutics, scientists at the Nemours Center for Childhood Cancer Research and the University of Delaware’s Materials Science and Engineering Department believe they have found a method in which nanotechnology can deliver chemotherapeutic agents to children without harming healthy cells, something which has generally eluded researchers in this field.
The focus of the study has been childhood leukemia. In the past nanoparticle-based drug delivery approaches in children have been poorly developed, because the focus has been on adult cancers. The research findingsconfirm that using nanotechnology has a major positive impact for targeting cancer cells: “Encapsulated dexamethasone (‘dex’) delivered to pre-clinical models with leukemia significantly improved quality of life and survival compared to the control receiving the unencapsulated drug.”
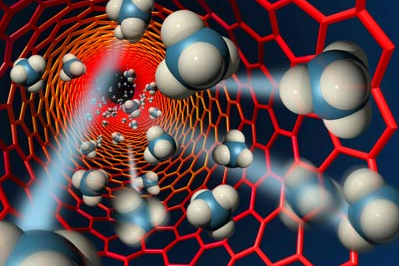
Nanoparticles have been emerging as a potentially viable class of cancer therapeutics for a number of years. The benefit of nanotechnology is that it uses encapsulated particles of drugs which are able to target the cell core. The nanoparticles can also effectively differentiate between cancer cells and normal cells.
A review in a 2007 edition of Nature Nanotechnology assessed the emerging platform nanocarriers offered for cancer therapy. Some of the early clinical results indicated that these materials can improve the effectiveness of the pharmaceuticals used and reduce side effects through the ability to more specifically target tumors and activate cellular uptake. The review discussed that a particular challenge lay in translating the basic research on novel nanoscale targeting approaches into the clinic setting.
The difficulty for pediatric cancer healthcare professionals is that the traditional drugs are not able to differentiate between healthy cells and cancerous cells. "There are currently seven or eight drugs that are used for chemotherapy to treat leukemia in children," points out Dr AyyappanRajasekaran, one of the lead authors of the research report. "They are all toxic and do their job by killing rapidly dividing cells." Issues such as secondary cancers and cognitive, hearing and developmental problems are a major concern for patients and their families.
In efforts to reduce these side effects and find a more effective transportation method, the scientists used polymeric nanoparticles containing chemotherapeutic agentsto provide controlled delivery of drugs to cancer cells in preclinical models. In these models of leukemia, Dr Rajasekaran and his team were able to improve survival and quality of life by using nanotechnology.
Additional benefits revealed by the research includes that by encapsulating the drug only a third of the typical dose is required and that the mice receiving drugs delivered by nanoparticles survived longer than those where the drugs were administered in the traditional manner.
This latest nanoparticle pharmaceutical research offers an important next step towards developing novel ways to deliver existing and affordable drugs to children with cancer.
